43 yr old male with complaints of abdominal distension and SOB since 15 days
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Case
Pt is a 43 yr old male with
chief complaints of abdominal distension and sob since 15 days.
HOPI
Pt was apparently asymptomatic 15 days ago then he developed abdominal bloating ,no regurgitation , discomfort is felt, aggravated after having food
Shortness of breath noted after having food ,on ordinary physical activity (grade 3 )
No h/o orthopnea ,chest pain, pnd , decreased urine output ,fever ,cough ,cold
K/c/o htn and dm 2 since 3 yrs
k/c/o alcoholic liver disease .
Personal history :
His educational status is inter completed and didn't go for further studies as he is not interested . Then he depended on his family for financial support upto 2013 ,then he joined finance based work did for 3 yrs then for raise in income he joined in wines shop management did for 4 yrs ,then he joined petrol bunk construction which he is currently working in
Daily routine.
His daily routine is waking up at 6am
Going for a walk 7 am
Getting ready and breakfast of idly/ dosa/ Vada and ready to work at 9 pm
Comes to home by 1 pm for having lunch
And went back to work 3pm and then he comes back at 8 pm for dinner and sleeps 9 pm. And consumes alcohol in the breaks for lunch and dinner and it causes late in work timings .
His family is upset with his alcohol consumption and he isn't violent or abusive towards them .
He got married in 2004
(Course of alcohol consumption)
After 3 yrs in family function and festival occasion he is used to have toddy 750 ml noticeably frequent in summer as seasonal commodity .
Then he started having beer 750 ml ,whisky 180 ml as per mood since 2010 due to influence of frnds and then continued due to pleasure .
As he was aware of consequences would have stopped intermittently for 1 month or so and then he would have started due to function and gathering and continued so ,due to his abdominal bloating ,uneasiness he used to stop .then due to chronic period of consumption he developed withdrawal symptoms of uneasiness, fearfulness ,sweating etc .
He had h/o trauma 3 yrs ago bike vs auto and had left thigh fracture and treated for it in our hospital
He got diagnosed with htn and diabetes during the period.
He then visited our hospital 3 months ago with complaints of vomiting later to find out alcoholic liver disease , he stopped consuming one month and then started on peer pressure and continued drinking
His last alcohol consumption is whisky 180 ml on 16/6/23. Then came to our hospital on 20/6/23 for c/o abdominal distension and vomitings similar to past visit to hospital.
General examination
Icterus present
No :
Pallor
Cyanosis
Clubbing
Lymphadenopathy
Oedema
Vitals
Temp:98.5°F
Bp: 120/80 mmhg
PR: 90 bpm
RR: 19 cpm
Systemic examination
Cvs :
Precordium normal
No thrills ,
On auscultation
S1,S2 heard ,no murmurs
CNS:
Higher mental functions :intact
Cranial nerves :intact
Motor system:Normal power,tone,Gait
Reflexes:normal
Sensory examination:Normal
No meningeal signs
Tremors : absent
Rs:
Shape of chest:Bilaterally symmetrical, Elliptical in shape
No visible chest deformities
No kyphoscoliosis,
Abdomino thoracic respiration, No irregular respiration
Trachea is central
Auscultation:
Normal vesicular breath sounds heard
P/A
INSPECTION:
Shape of abdomen:Distended
Umbilicus:inverted
Skin over the abdomen is shiny
All quadrants are moving equally with respiration
No visible peristalsis, Hernial orifices intact
Visible superficial abdominal vein running vertically down is seen
External genitalia normal
PALPATION:
Temperature:Not raised
Tenderness:Absent
No Rebound tenderness
No guarding rigidity
Mild Hepatomegaly
Percussion
No shifting dullness ,
No fluid thrill
Auscultation
Bowel sounds are heard.
Diagnosis
Alcoholic liver disease with alcoholic dependency syndrome
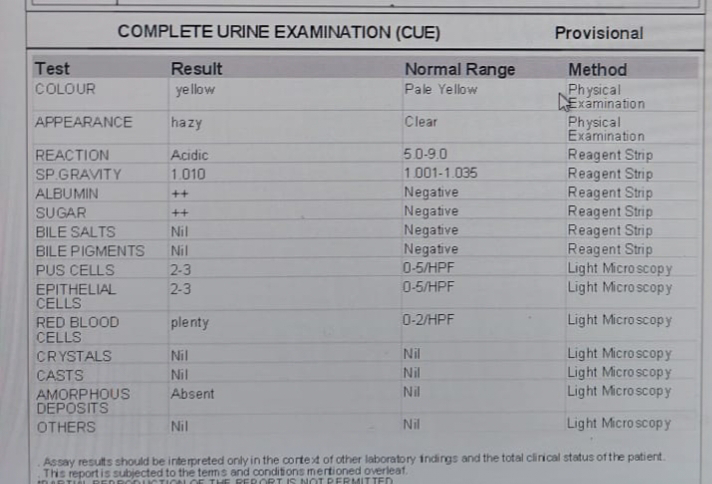
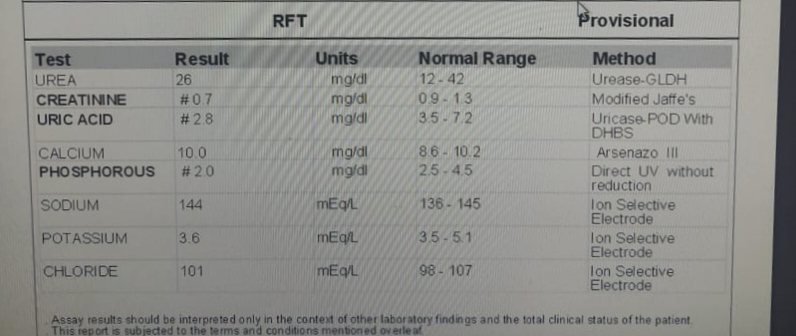
Investigations on 20/6/23
FBS - 173 mg/dl
Plbs - 258 mg /dl
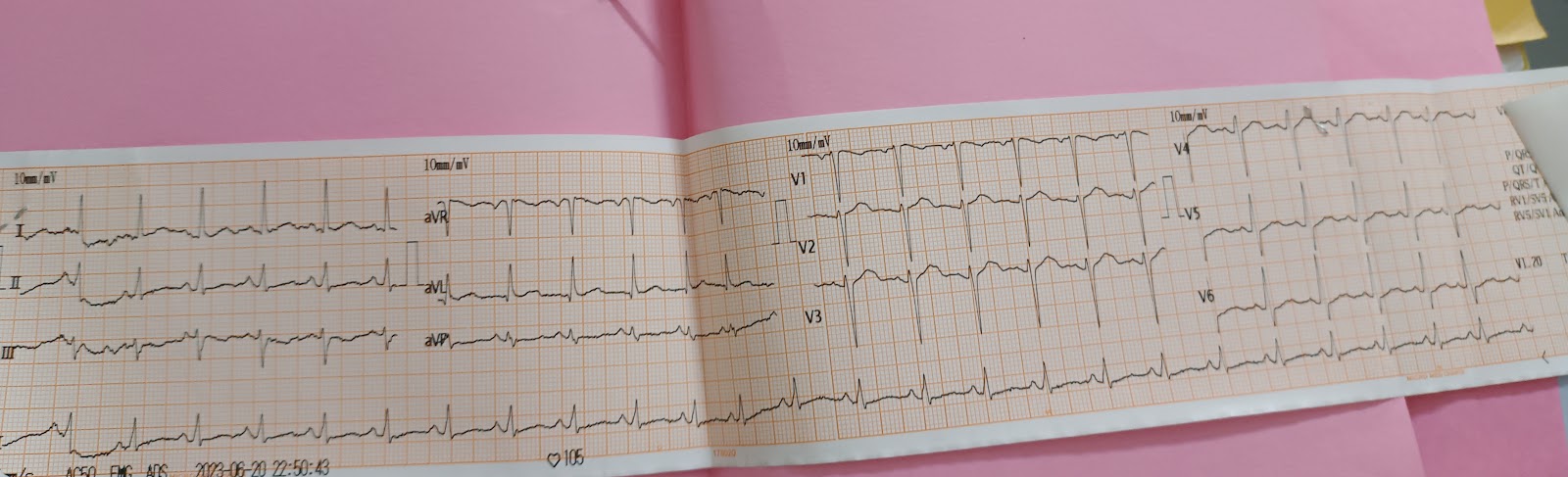
ECG
On 22/6/23
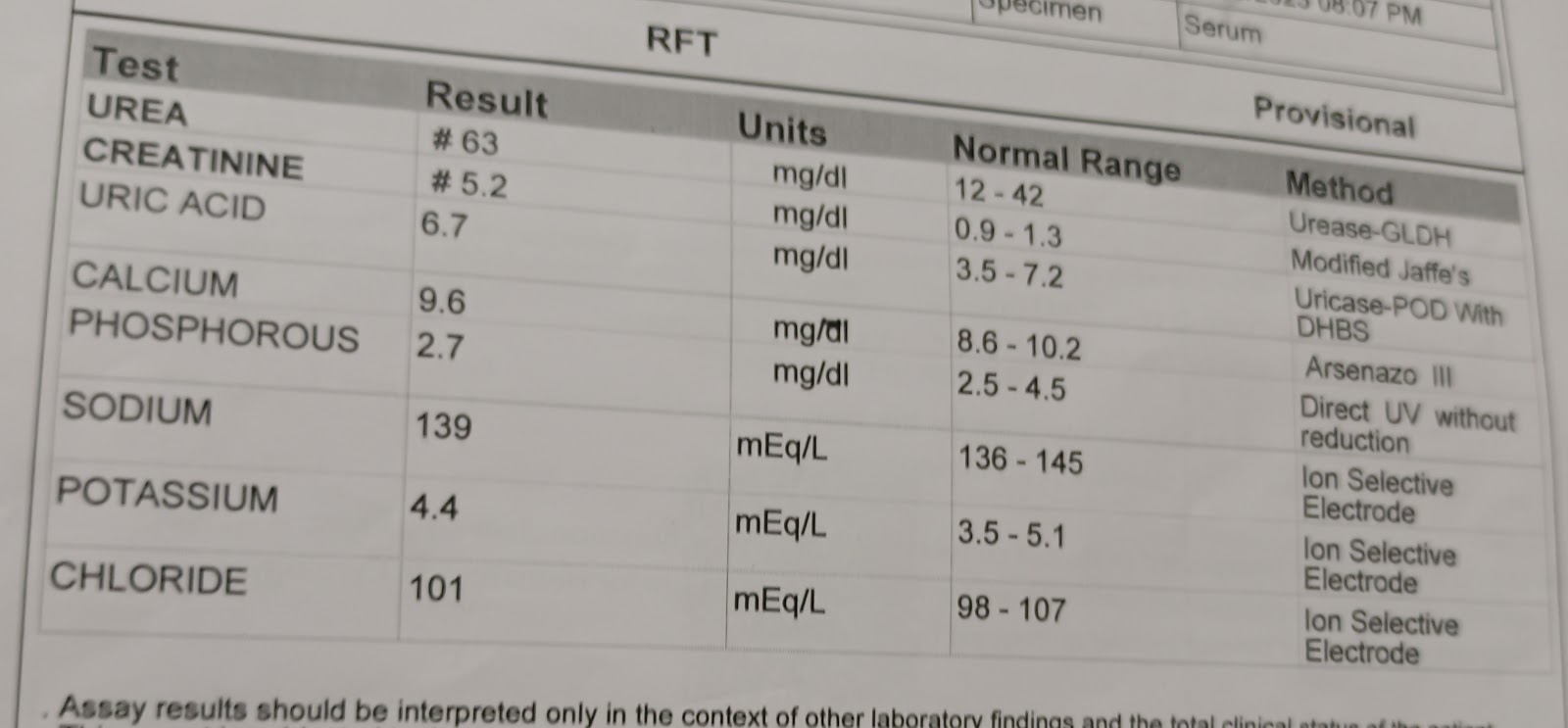
On 23/6/23
Gastrology referral
Endoscopy done
Esophagyus :small hiatus hernia ,no varices ,grade D esophageal reflux disease
Stomach : no blood seen ,diffuse gastritis
Duodenum :d2 normal ,smooth globular extrinsic impression in d1 likely to be gb compression
Advice
Strict alcohol abstinence
On 23/6/23
Psychiatry referral
Impression : alcoholic dependence syndrome. Currently abstinence
1.Tab .PAN 40 MG PO /OD
2.SYP.LACTULOSE PO/OD (9PM)
3TAB .GLIMI M1 PO OD 8AM
4.TAB . AMLODIPINE PO/OD 8 AM
5. TAB .LORAZEPAM 2 MG x 1 week
6.TAB .BACLOFEN XL 20 MG x. 1 week
7.TAB .BENFOTHIAMINE 100 MG x 1 week
8. TAB.UDILIV 300 MG PO/BD
9.TAB.BEFLEX FORTE PO/OD x 1 week
10.SYP .HEPAMERZ 15 ML PO/TID x 1 week
Patient got discharged after explaining the alcoholic effects and medication mentioned above on 24/6/23.