41 yr male patient with left loin pain
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
A 41 year old male patient who is a resident of ismapelli plumber by occupation came to the opd with
CHIEF COMPLIANTS:-
1.fever since 4 days
2.left loin pain since 4 days
HISTORY OF PRESENT ILLNESS:-
patient was apparently asymptomatic 6 months back then he developed loin pain ( cause unknown) went to a local hospital and got treated ( treatment given -unknown) .
then 4 days back he developed fever which was continuous high grade not associated with chills ,rigor, convulsions and skin rash.and not relieved on medication (dolo) after which he had 2 episodes of vomiting which is non projectile and non bilious .
he had pain in left lumbar region since 4 days which is dragging type of pain insidious in onset with no aggravating and relieving factors .
No history of hematuria , anuria, polyuria, incontinence, swelling of legs, breathless ness , nocturia.
past history:-
diabetic ( type 2) since 10 years under medication and is under control.
medication (oral drugs- name and dose unknown)
not a known case of HTN , epilepsy, CAD , asthma ,TB ,leprosy
personal history:-
appetite - normal
diet - mixed
bowel and bladder - regular
sleep adequate - adequate
addictions - occasionally alcohol
Daily routine:-
patient was a plumber of 41 year old
events in life:- when he was 25 that is 16 years back he was married. After 3 years of marriage he went to hospital for infertility and some medication was taken ( medication included both herbal and generic) which he used for 6 months continuously and then irregularly for 7 years .
10 years back he went to a hospital for general checkup where he got diagnosed with DM (type 2) and is taking medication since then.
FAMILY HISTORY:-
no significant family history
Allergic history:-
not allergic to any kind of drugs or food.
GENERAL EXAMINATION:-
patient is conscious , coherent , co operative and well oriented towards time place and person.
:well bulit and well nourished
:no pallor, icterus ,cyanosis, clubbing, lymphadenopathy and edema.
VITALS :-
temperature:-Afebrile
pulse rate :-74 bpm
respiratory rate:-20 cpm
B.P :-130/80 mm Hg
GRBS:- 204 mg%
SYSTEMIC EXAMINATION:-
CVS :- S1; S2 heard ; no murmurs
Respiratory system:- Bilateral air entry present, normal vesicular breath sounds are heard all over the chest
Per abdomen:- soft , non tender.
CNS :- no focal deformities,tone normal
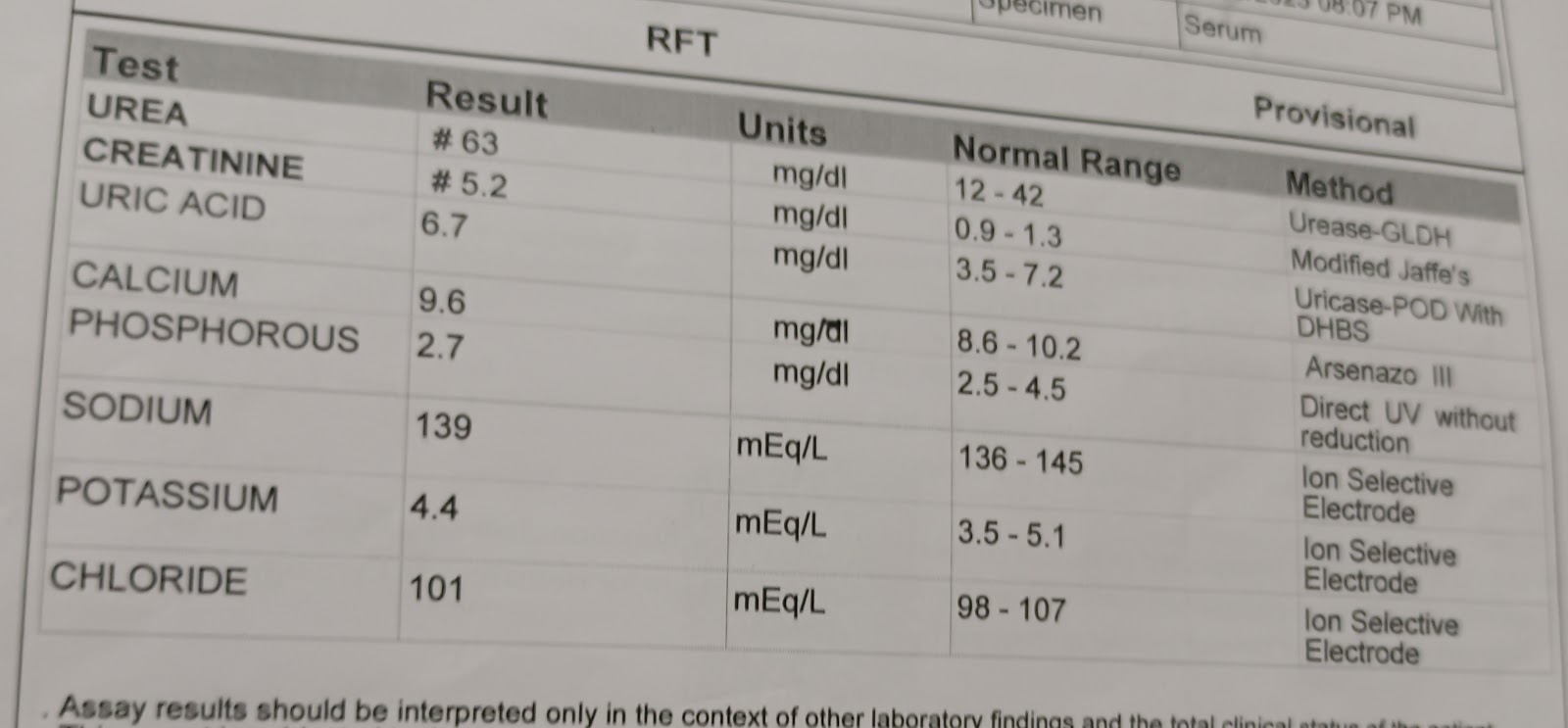
INVESTIGATIONS :-
ELECTROLYTES:-
SERUM CREATININE:-on 12/07/22 is 7.0 mg/dl