This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
Case
A 23 yr old male patient who is resident of nakrekal,gold smith by occupation,presented to our hospital with
Chief complaints of backache since 5 days and vomiting on 1/12/22 afternoon
History of presenting illness:
Patient presented with backache since 5 days which is insidious in onset and gradually progressive,continous and had fever for 2days at the onset of the backache which is high grade associated with mild chills and rigor,
sweating is noticed and treated at their local hospital for the same and reduced from 108°F to 102°F ,reduced further {couldn't register as lack of record and noted of patients knowledge} and now patient is afebrile .
He had vomiting, on 1/12/22 afternoon which is of one episode , non bilious,non projectile ,food as content he took ,
He has abdominal pain since then,
He complains of black colored stools on 1/12/22 ,not associated with blood,non foul smelling
No history of petechiae and abdominal distension
No history of burning micturition an decreased Volume and frequency of urine.
Daily routine
He wakes up around 7am and has breakfast around 8 am commonly idli on daily basis and gets to work at 10 am with lunch as rice and curries at 1pm and gets off work around 8pm and has dinner at 9pm rice /chapatis .
His diet is mostly vegetarian and very occasionally non veg,
Appetite is normal
Sleep is inadequate these days due to back ache and abdominal pain
Bowel shows certain changes as described of today
Addictions being occasional consumption of alcohol {beer of 1or 2 bottles}
Past history
No history of any similar complaints in past.
Ho history of Diabetes,hypertension,asthma,epilepsy, tuberculosis.
No history of previous surgeries and prolonged hospital stay
Treatment history
He is been taking paracetamol 650 mg bd for 3 days.
Family history
Not significant
General examination
Patient is conscious ,coherent and co operative.
Moderately built and moderately nourished.
Pallor :no
Icterus:no
Cyanosis
Clubbing
Lymphadenopathy
Edema
Are absent
Vitals
Temperature : afebrile
Blood pressure : 110/80 mm Hg
Pulse rate :82 bpm
Respiratory rate :16 cpm
SYSTEM EXAMINATION:
Abdominal examination-
INSPECTION
On Inspection Abdomen is flat, no abdominal distension, umbilicus is central and inverted ,no engorged veins,no scars,sinuses,hernial ornifices are clear
PALPATION
All inspectory findings are confirmed on palpation
No tenderness is seen .
No hepatomegaly and splenomegaly.
PERCUSSION : No significant findings
AUSCULTATION: bowel sounds heard
RESPIRATORY EXAMINATION
trachea central,
normal respiratory movements,
normal vesicular breath sounds.
CARDIOVASCULAR SYSTEM EXAMINATION
S1 ,S2 heard ,no murmurs
CNS EXAMINATION
No focal neurological deficits
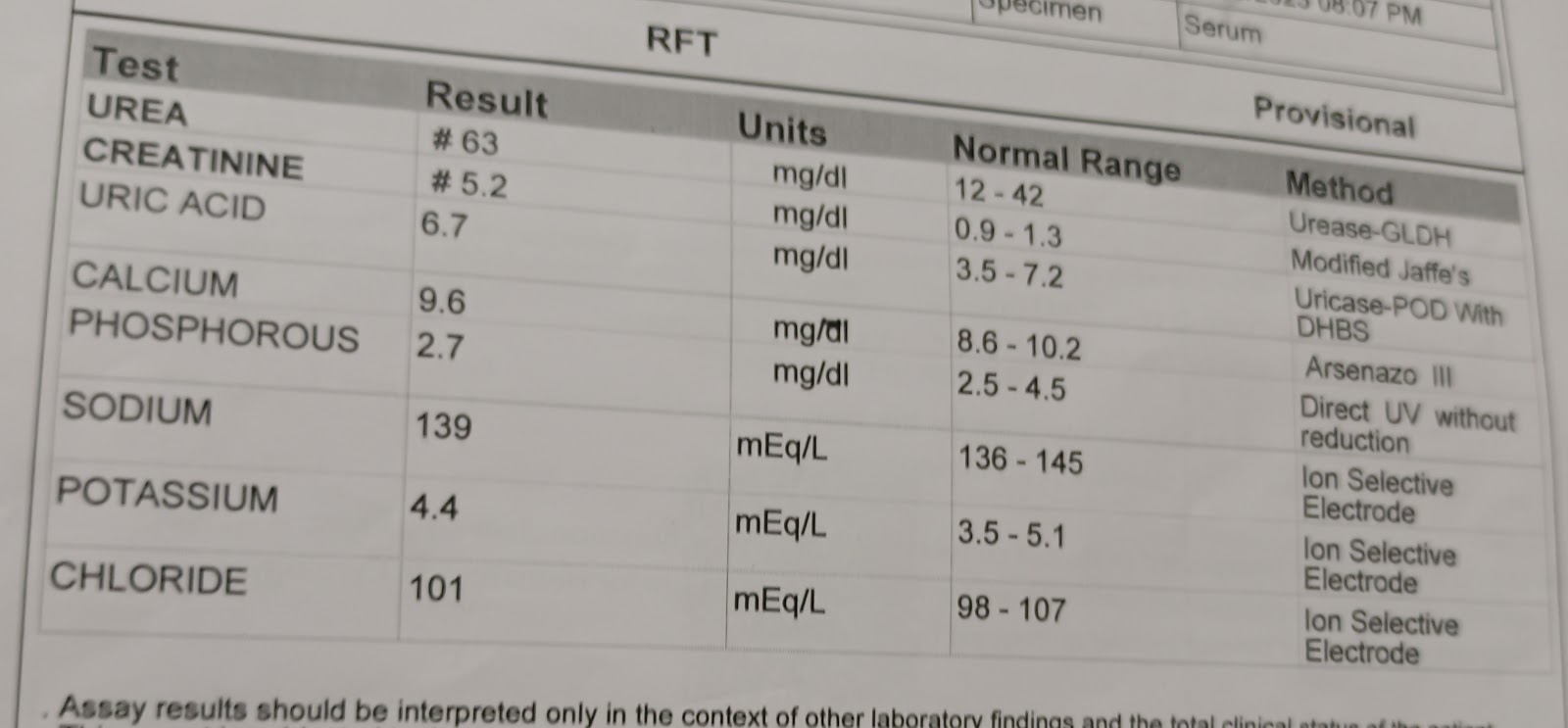
INVESTIGATIONS
IN Previous hospital
Hematological tests- on 30/11/22
Platelet count -81,000 /cumm
Tests for dengue antibodies
Ig G and IgM non reactive
And dengue NS1 antigen Is reactive
On 1/12/22
Platelet count -37,000/ cumm
Would like to investigate for
Hemogram
Complete urine examination
Liver function tests
Serum creatinine and urea
Serum electrolyte
ECG
Usg abdomen
Chest X-ray
PROVISONAL DIAGNOSIS
DENGUE WITH THROMBOCYTOPENIA
TREATMENT
IV FLUIDS. NS,RL 500ML
INJ NEOMOL IV / SOS {TEMP >100°F}
TAB DOLO 650mg PO/BD
INJ ZOFER 4mg IV/ OD
INJ PANTOP 40 mg IV /OD