21yr old female with fever.
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE-IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT. HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH A SERIES OF INPUTS FROM THE AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE-BASED INPUT
Case
21 year old female patient from Ismail palli, who is a Bsc nursing student ,came to the casuality with chief complaints of
•Fever since 21/7/22
•Body pains
•Vomitings since 21/7/22 evening
•non-productive cough
HOPI :
The patient presented with fever which is insidious in onset,high grade,continous,associated with chills&body pain since 10 am 21/7/22
H/o Vomitings on 21/7/22 evening 6 episodes , non bilious type,non-projectile, food particles and water as content,was associated with abdominal pain(h/o Outside food intake - corn,chicken on 20/7/22)
No H/o loose stools
No H/o burning micturation,shortness of breath,chest pain,palpitations,diarrhoea.
Daily routine :
Wakes up at 7 am,do her regular activities,have breakfast and attend college classes,clinicals,have lunch at 1pm and attend college from 2-4pm , and having snacks on road side frequently, goes to bed at 10pm
Past history :
Not a known case of diabetes/ hypertension/asthma/CAD/CVA/Epilepsy/Typhoid/Thyroid disorders
No previous surgical history.
Personal history :
•Diet : mixed
•Appetite : decreased since the fever
•Sleep : distributed sleep because of chills and rigor
•Bowel movements :
Vomitings
•Bladder movements: Regular
•Addictions : None
Allergies :
Allergic to potato , Roselle leaves and brinjal
Family history : not significant
Menstrual history :
Age of menarche : 12
Duration of mensuration : 5 days
LMP : 25/6/22
Regular : 5/30
No other Gynecologic problems
Immunization status :
Vaccinated up to date
Vaccinated for covid -19
GENERAL EXAMINATION •Patient is examined in a well lit room after obtaining consent
•Patient is conscious, coherent, cooperative.
Well built and well nourished.
•Height -5'2
• Weight - 55 kgs
•Pallor , Icterus,clubbing, cyanosis, koilonychia, edema are absent
VITALS :
Temp- 100f
Bp-100/80 mm hg
PR- 84bpm
RR-16CPM
Spo2- 99% on RA
GRBS : 102
SYSTEMIC EXAMINATION
RS-. bilateral air entry present
CVS : S1, S2 + no murmurs
P/A- soft and non tender
bowel sounds present
CNS :. No focal neurological defeicit
HMF intact
Power in B/L upper and lower limb Is 5
Reflexes are present with B/L plantars and flexors
INVESTIGATIONS :
On 22/7/22
On 24/7/22"
*Haemogram
6 : 30 am
"On 25/7/22"
*Hemogram
(9 am)
(7pm)
*Record of Temparature,BP, RR AND SPO2
*USG Abdomen
On 26/7/22"
*Haemogram
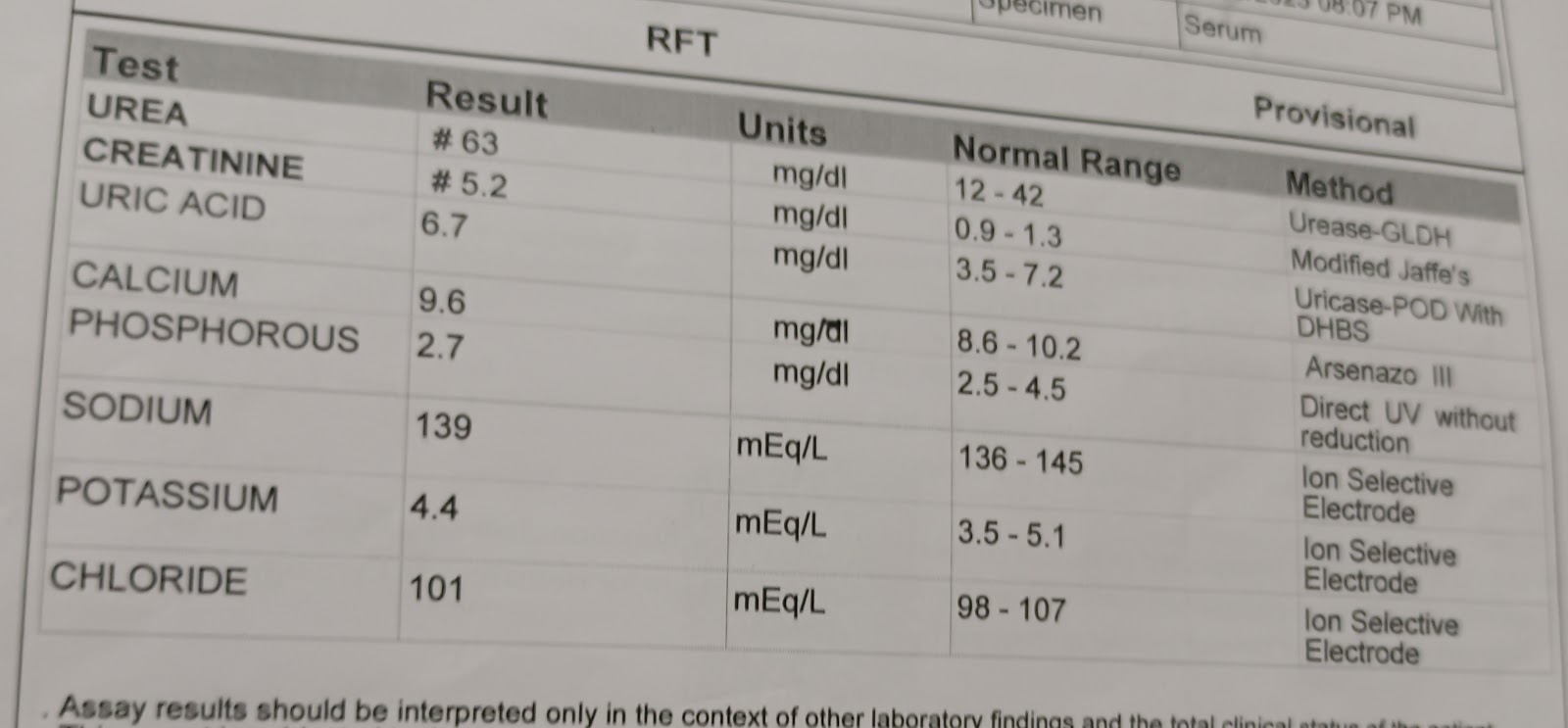
*Blood Urea
*Serum Creatinine
*Serum electrolytes & Serum Iodized Calcium
"On 27/7/22"
*Haemogram
Fever chart
Xray
PROVISIONAL DIAGNOSIS :
• DENGUE WITH THROMBOCYTOPENIA AND LEUCOPENIA
*TREATMENT : :Plenty of oral fluids
IVF ( NORMAL SALINE , RINGER LACTATE )
75 ml / hr
Inj Xone 1gm IV /BD
Inj Mifenac MR PO / BD
Tablet okacet PO/BD
Tablet Doxy 100mg/PO/BD
Tablet metaspas PO / BD
Inj Neomol IV /SOS
Tablet PCM 600mg PO/TID