1801006060 - LONG CASE
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
A 50 year old male patient farmer by occupation came to the department with
chief complaints :
- shortness of breath since 10 days
- complaints of edema in both upper and lower limbs since 6 days
decreased urine output since 6 days
History of presenting illness :
Patient was apparently asymptomatic 1yr back ,then he noticed swelling in both the legs and on consultation diagnosed with chronic kidney disease and started on medication which was taken irregularly for subsiding the symptoms
From then on he intermittently have pedal edema and shortness of breath .
In 2023 Jan he developed shortness of breath grade 3 and he was rushed to a hospital; and said to have heart ; lung and kindney functional abnormalities; and was admitted in the hospital for 2 weeks , where they gave some medication, but he did not use properly and symptoms persisted .
10 days back he had sudden onset of shortness of breath which is GRADE IV, orthopnea
Edema of both upper and lower limbs since 6 days which is pitting type (grade 4 )upto thigh .
PAST HISTORY:-
H/O fall from tree in 2008 lead to back ache and headache with use of Nsaids
DM since 6 yrs ( metformin is being used )
He is diagnosed with Tuberculosis 4yrs back and treated with antitubercular therapy
Not a known case of ; Hypertension, thyroid, Asthma .
No history of any surgeries in the past.
Drug history:- intermittent use of NSAIDS from past 14 years .
ATT used for tb
PERSONAL HISTORY:-
Diet - mixed
Appetite normal
Sleep - adequate
Bowel - regular; decreased urinary output since 6 days
Addictions - occasionally alcohol consumption
Cigarette stopped 25 years back before 1 pack per year.
Daily routine
He is farmer by occupation and used to go to work by waking up at 6 am and breakfast at 7 am ,completes work by afternoon ,takes rest and has dinner at 8 pm ,sleep at 10pm
He stayed at home since the fall from tree due to low backache
FAMILY HISTORY:-
no significant family history
ALLERGIC HISTORY:-
no allergies to any kind of drugs or food items
GENERAL EXAMINATION:-
Patient is conscious, coherent, and cooperative
Well built and well nourished
No pallor
No icterus
No cyanosis
No clubbing
No lymphadenopathy
Pitting edema seen in both lower limbs
imaginary pillow
Vitals*
Pulse rate : 85 bpmRate, rhythm(regular)character(normal ), volume - normal
peripheral pulsations [Carotid, brachial, radial, femoral, popliteal, posterior tibial, dorsalis pedis]- present
no radio radial delay
BP: 120/80 mm Hg measured on Rt Upper arm In the supine position
Respiratory Rate:25 CPM;
type- thoracic abdominal
Temperature:- 96.9 F
SPO 2 :- 98 %
GRBS :- 136 mg/dl
SYSTEMIC EXAMINATION
CARDIOVASCULAR SYSTEM :-
INSPECTION:-
Appears normal in shape
Apex beat is not visible
No Dilated veins, scars, sinuses
PALPATION:
1- All inspector findings were confirmed.
2-Trachea is central.
No palpable murmurs (thrills)
PERCUSSION:-
Heart borders are normal limits .
AUSCULTATION:-
S1 AND S2 HEARD.
APEX BEAT @ 6TH INTERCOSTAL SPACE IN ANTERIOR AXILLARY LINE
P2 NOT PALPABLE
JVP MILD RAISE
RESPIRATORY SYSTEM:-
Inspection shape of chest normal
Bilateral airway entry - present
Percussion Right Left
Infra clavicular: resonant resonant
Mammary: resonant dull
Axillary: resonant dull
Infra axillary: resonant dull
Supra scapular: resonant resonant
Infra scapular: resonant dull
Inter scapular: resonant dull
Auscultation: Right. Left
Supra clavicular:. NVBS NVBS
Infra clavicular: NVBS NVBS
Mammary: NVBS decreased
Axillary: NVBS decreased
Infra axillary: NVBS decreased
Supra scapular: NVBS NVBS
Infra scapular: NVBS decreased
Inter scapular: NVBS decreased
PER ABDOMEN:-
no tenderness
no palpable organs
bowel sounds - present
CNS EXAMINATION:-
The patient is conscious.
No focal deformities.
Signs of meningeal irritation:-
NEGATIVE
cranial nerves - intact
sensory system - intact
motor system - intact
INVESTIGATIONS:-
On 13/3/23 :-
Serology:
HIV : NEGATIVE
Anti HCV antibodies:- NON REACTIVE
HbsAg :- NEGATIVE
RANDOM BLOOD SUGAR: 125mg/dl
CUE :- NORMAL
S.UREA: 64mg/dl (N:- 12-42mg/dl)
S. CREATININE: 4.3 mg/dl
S. Na+: 138
S. K+: 3.4 (3.5-5.5)
S. Cl-: 104
CBP :-
Hb :- 12.6 gm/dl
HbA1C: 6.5%
FASTING BLOOD SUGAR :- 93 mg/dl
POST LUNCH BLOOD SUGAR :- 152 mg/dl
15/3/22 :-
CBP :-
Hb :- 11.7 Gm/dl
MCH :- decreased
Blood urea :- 140 mg/dl
serum creatinine:- 5.7
Serum electrolytes:- potassium- 3.0 mEq/L
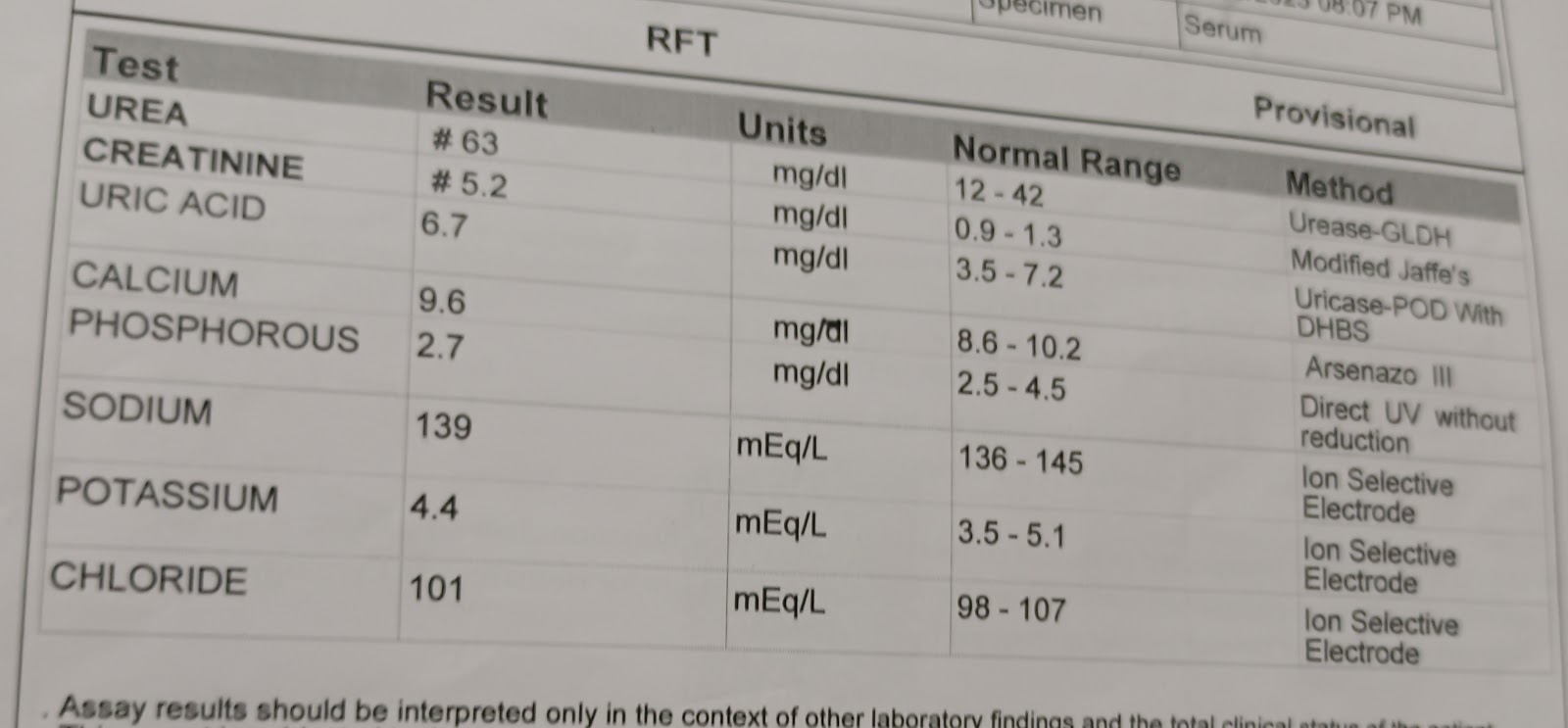
On 16 /3/23
Serum creatinine :5.9{0.9-1.3 mg/dl}
Hemogram
Hemoglobin #11.4gm/dl
Lymphocytes #18%
PCV #35.7
MCH -#26.7
RDW-CV #19.6%
RBC COUNT - 4.27 MILLION/CUMM
BLOOD UREA -191 mg/dl {12-42}
Serum electrolyte
Potassium #3.1 {3.5-5.1}
Chest X Ray
2D echo
MODERATE MR+: MODERATE TR+ WITH PAH: TRIVIAL ECCENTRIC TR+
GLOBAL HYPOKINETIC, NO AS/MS. SCLEROTIC
MODERATE LV DYSFUNCTION+
DIASTOLIC DYSFUNCTION PRESENT
ULTRASOUND:
USG CHEST:
IMPRESSION:
BILATERAL PLEURAL EFFUSION (RIGHT MORE THAN LEFT) WITH UNDERLYING COLLAPSE.
USG ABDOMEN AND PELVIS:
MILD TO MODERATE ASCITES
RAISED ECHOGENECITY OF BILATERAL KIDNEYS
DIAGNOSIS:-
HEART FAILURE WITH reduced EJECTION FRACTION
WITH ACUTE KIDNEY INJURY ON CHRONIC KIDNEY DISEASE (SECONDARY TO DIABETES/NSAID INDUCED)
WITH K/C/O DM II SINCE 6 YEARS
WITh TB 3 years ago